COBRA administration made simple.
Keeping up with compliance requirements can be a challenge. Between tracking timelines, generating notices, applying subsidies, collecting payments, managing eligibility, communicating with carriers, and staying current with the legislation, things start to get confusing.
COBRA administration made simple.
Keeping up with compliance requirements can be a challenge. Between tracking timelines, generating notices, applying subsidies, collecting payments, managing eligibility, communicating with carriers, and staying current with the legislation, things start to get confusing.
We’re here to tame the chaos for you.
COBRA administration made simple.
Keeping up with compliance requirements can be a challenge. Between tracking timelines, generating notices, applying subsidies, collecting payments, managing eligibility, communicating with carriers, and staying current with the legislation, things start to get confusing.

We’re here to tame the chaos for you.
We’re here to tame the chaos for you.
-
Notices & Communications
-
Eligibility Management
-
Payment Processing
Streamline COBRA Administration with our Full-Service Solution
We're hands on, so you can be hands off.
Make COBRA administration a breeze all year long with a full service solution that helps keep you in compliance with timelines and regulations. You’ll be left with less stress, more time, and most importantly…peace of mind.
Streamline COBRA Administration with our Full-Service Solution
We're hands on, so you can be hands off
Make COBRA administration a breeze all year long with a full service solution that helps keep you in compliance with timelines and regulations. You’ll be left with less stress, more time, and most importantly…peace of mind.
Streamline COBRA Administration with our Full-Service Solution
We're hands on, so you can be hands off
Make COBRA administration a breeze all year long with a full service solution that helps keep you in compliance with timelines and regulations. You’ll be left with less stress, more time, and most importantly…peace of mind.
Support throughout the entire COBRA lifecycle
- Compliance with federal and state regulations
- Monitor qualifying events for all COBRA-eligibles
- Generation & mail fulfillment of required notices
- Eligibility maintenance
- Enrollment processing with carriers
- Coverage extensions & terminations
- Collection of premium payments
- Tracking for subsidized premiums
- Monthly employer remittance
- Compliance with federal and state regulations
- Monitor qualifying events for all COBRA-eligibles
- Generation & mail fulfillment of required notices
- Eligibility maintenance
- Enrollment processing with carriers
- Coverage extensions & terminations
- Collection of premium payments
- Tracking for subsidized premiums
- Monthly employer remittance
- Compliance with federal and state regulations
- Monitor qualifying events for all COBRA-eligibles
- Generation & mail fulfillment of required notices
- Eligibility maintenance
- Enrollment processing with carriers
- Coverage extensions & terminations
- Collection of premium payments
- Tracking for subsidized premiums
- Monthly employer remittance
Member support
Call center and email support is available to participants, making it easy to get quick answers and guidance on how to enroll, make payments, and more.
“
In this ``just doing my job`` world of mediocrity, the ebm team gives the world hope that there are still those out there who care and truly believe in providing superior customer service.
-COBRA participant

Member Support
Call center and email support is available to participants, making it easy to get quick answers and guidance on how to enroll, make payments, and more.
“
In this “just doing my job” world of mediocrity, the ebm team gives the world hope that there are still those out there who care and truly believe in providing superior customer service.

Convenient, secure access to your data:
Member portal
- View copies of mailed communications
- Enroll in coverage
- Manage and make payments
Employer portal
- View member status, plans, and payments
- Access generated communications and historical data
- Retrieve participant data and reports
Broker portal
- Access COBRA in the cloud across your book of business
- View detailed plan and member information
- Generate reports by client
Convenient, secure access to your data:
Member portal
- View copies of mailed communications
- Enroll in coverage
- Manage and make payments
Employer portal
- View member status, plans, and payments
- Access generated communications and historical data
- Retrieve participant data and reports
Broker portal
- Access COBRA in the cloud across your book of business
- View detailed plan and member information
- Generate reports by client
Convenient, secure access to your data:
Member portal
- View copies of mailed communications
- Enroll in coverage
- Manage and make payments
Employer portal
- View member status, plans, and payments
- Access generated communications and historical data
- Retrieve participant data and reports
Broker portal
- Access COBRA in the cloud across your book of business
- View detailed plan and member information
- Generate reports by client
Advantages of Working With ebm
Employers
With so many requirements, things get complicated. Our team of experts help you navigate the complex. We remove the guesswork and automate processes with industry-leading technology.
- Meet Department of Labor (DOL) guidelines: Our system automates tracking of COBRA timelines and generates and mails all required notices
- Streamline enrollment and eligibility: We eliminate manual work by managing enrollment and coverage updates with your carriers
Participants
Participants can login to the portal to access copies of all mailed notices and communications, elect or waive their coverage, and make payments.
- Accessible portal: Our mobile-response portal makes it easy for employees to access their account and make elections and payments anytime, anywhere.
- Convenient payment options: Employees can pay however they want. Whether it’s a credit card, debit card, ACH, or even a check.
Brokers
- Provide a better experience for your clients: Enhance the experience for your clients by providing a user-friendly, mobile-optimized COBRA portal that automates tracking of timelines, enrollment, and eligibility management.
- Leverage our team of experts: Our team of experts has deep knowledge of COBRA compliance and current legislation. We’ll help keep your clients in compliance and their employees covered.
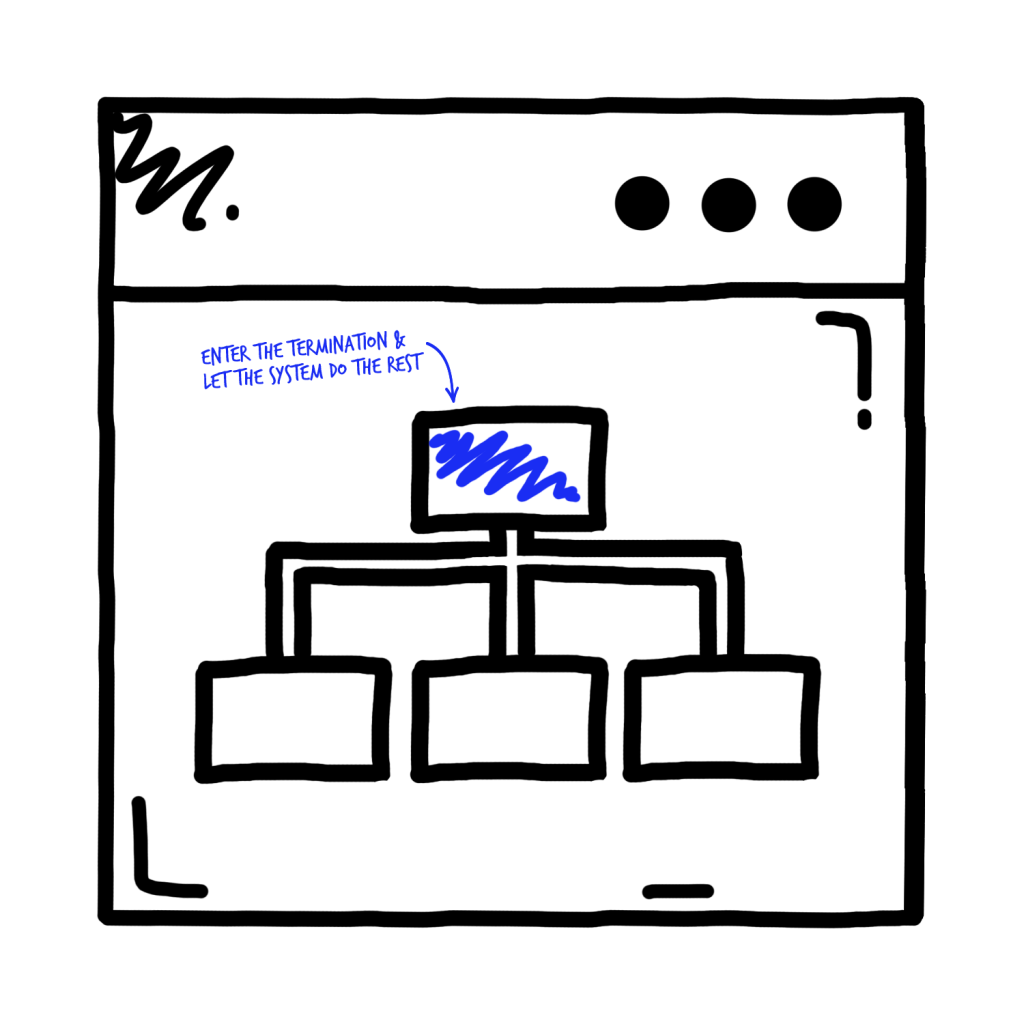
Explore our platforms
Seamlessly administer benefits across all of your populations.
When you’re using any of our enrollment platforms, you benefit from a straightforward workflow as employees gain and lose eligibility: what was once a multi-step process is streamlined into one step. By simply terminating an employee within the platform, the COBRA process is automatically triggered and the timeline begins.
Explore our platforms
Seamlessly administer benefits across all of your populations
When you’re using any of our enrollment platforms, you benefit from a straightforward workflow as employees gain and lose eligibility: what was once a multi-step process is streamlined into one step. By simply terminating an employee within the platform, the COBRA process is automatically triggered and the timeline begins.
COBRA Administration the ebm way
Our unique approach to COBRA administration is a blend of cutting-edge technology, industry-leading expertise, and outstanding customer service.
Tech-Driven Efficiency
ebm simplifies the management of COBRA-eligible beneficiaries, ensuring timely notifications and accurate tracking of election periods. Our system takes the guesswork out of the process, providing you with automated reporting and audit trails for effortless compliance.
Exceptional Client Service
We don’t just administer COBRA—we build relationships. Our dedicated support team is available to address questions, alleviate concerns, and ensure a seamless COBRA administration experience. Whether it’s a question about a timeline, enrollment and eligibility, or how to use our software, we’re here for you – and your employees.
Keeping in compliance has never been simpler
HR and benefits administration comes with so many challenges, but navigating the complexities of COBRA administration doesn’t have to be one of them. At ebm, we believe in easing your burden so that you can focus on what truly matters: your people. We do the heavy lifting, while you enjoy streamlined workflows and an unparalleled user experience.
Streamlined COBRA administration
We understand the challenges you face, and we’re here to help transform these complexities into an organized, simplified process.
Our advanced technology platform automates critical tasks to ensure your COBRA administration process aligns with regulatory requirements. From initial notifications to tracking of election periods and premium payments, we handle it all, minimizing the risk of non-compliance and penalties.
HR teams are known for their people skills, and we believe you should expect the same from your COBRA administration provider. Our support doesn’t stop at software. We ensure you have a dedicated representative to address your questions, provide timely updates, and offer support whenever needed.
Streamlined COBRA administration from ebm – it’s more than just a service, it’s a strategic asset for your HR team. Join the ranks of the many organizations who have transformed their COBRA administration process with ebm.
FAQs on COBRA Administration
What is the Consolidated Omnibus Budget Reconciliation Act (COBRA)?
The Consolidated Omnibus Budget Reconciliation Act, more commonly known as COBRA, is a federal law enacted in 1985 that allows eligible employees and their dependents to continue health insurance coverage at group rates in certain instances where coverage might otherwise end, such as job loss, reduction in work hours, or certain life events.
What does a COBRA Administrator do?
COBRA administrators oversee the tracking and management of healthcare benefits continuity for employees losing access to health coverage due to a qualifying event. This includes notifying participants of their rights via distribution of required notices, processing enrollment, collecting premiums, and maintaining eligibility with insurance carriers.
How does COBRA Administration work?
COBRA Administration involves managing all aspects of an organization’s COBRA compliance. It starts with notifying eligible employees about their rights and responsibilities under COBRA. The administrator then tracks elections, oversees premium payments, ensures the continuation of health coverage with insurance providers, and maintains regulatory compliance and records. In essence, COBRA administration is about ensuring that the organization meets its legal obligations under COBRA and that eligible employees can access their right to continued healthcare coverage.
How to get started with COBRA Administration Services
To start with COBRA administration services through ebm, get in touch with our team. We’ll guide you through our process and discuss your organization’s specific needs.
Who qualifies for COBRA?
COBRA coverage is available to employees, their spouses, and dependent children when group health insurance could otherwise be lost due to specific events, known as qualifying events. These include job loss (voluntary or involuntary, except for cases of gross misconduct), reduction in work hours, divorce or legal separation, death of the covered employee, or a dependent child losing their dependent status under the plan.
Eligibility for COBRA benefits
Eligibility for COBRA benefits extends to employees and their families covered under the employer’s group health plan on the day before a qualifying event occurs. Qualifying events include job loss, reduction in work hours, death, divorce, or a dependent losing their status under the plan. The individual must also be able to continue participation in the group health plan to be eligible.
Who must comply with COBRA?
COBRA applies to all private-sector group health plans maintained by employers that had at least 20 employees on more than 50 percent of its typical business days in the previous calendar year. Both full and part-time employees are counted to determine whether a plan is subject to COBRA.
Penalties for non-compliance with COBRA
Non-compliance with COBRA can result in substantial penalties, including excise tax penalties for each violation and an ERISA statutory penalty.
How long does COBRA coverage last?
COBRA coverage typically lasts for 18 months or 36 months following the qualifying event. This timeline depends on the type of qualifying event, and may vary based on specific situations and regulatory changes.
Take back your peace of mind.
Start leveraging our full suite of solutions today.